Arthritis of the Knee

Arthritis is one of the most common causes of persistent pain of the knee joint. Pain, swelling, and stiffness are the primary symptoms of arthritis. Any joint in the body may be affected by the disease, but it is particularly common in the knee. Knee arthritis can make it hard to do many everyday activities, such as walking or climbing stairs. It is a major cause of lost work time and a serious disability for many people. Although there is no cure for arthritis, there are many treatment options available to help manage pain and keep people staying active.
Causes of Knee Pain and Arthritis
Many causes and forms of arthritis exist; they can be divided into a few categories:
- Osteoarthritis (OA). OA is by far the most common type of knee arthritis. This is an age-related "wear and tear" type of arthritis. It usually occurs in people 50 years of age and older and often in individuals with a family history of arthritis. The cartilage cushioning the bones in the knee wears away. The bones then rub against each other, causing hip pain and stiffness. Osteoarthritis may also be accelerated or affected by old injuries and even the alignment of your leg.
- Rheumatoid arthritis (RA) / “Inflammatory Arthritis”. RA is an autoimmune disease in which the synovial membrane becomes inflamed and thickened. This chronic inflammation can damage the cartilage, leading to pain and stiffness. Rheumatoid arthritis is the most common type of a group of disorders termed "inflammatory” or “autoimmune” arthritis.
- Post-traumatic arthritis. This can follow a serious knee injury or fracture. Meniscal tears and ligament injuries can cause instability and additional wear on the knee joint, which over time can result in arthritis. The cartilage can become damaged or overloaded and lead to knee pain and stiffness over time.
Anatomy
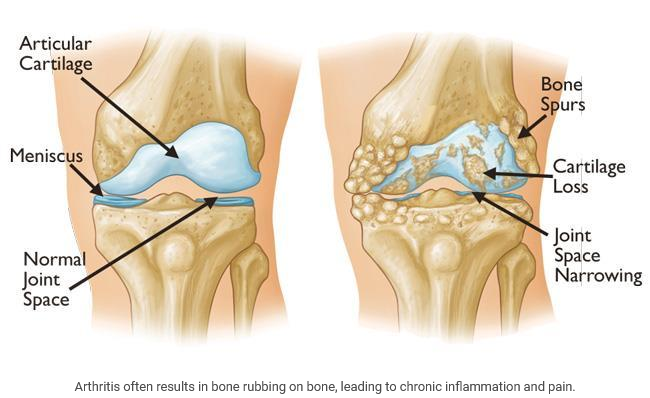
The knee is the largest and strongest joint in your body. It is made up of the lower end of the femur (thighbone), the upper end of the tibia (shinbone), and the patella (kneecap). The ends of the three bones where they touch are covered with articular cartilage, a smooth, slippery substance that protects and cushions the bones as you bend and straighten your knee.
Two wedge-shaped pieces of cartilage called meniscus act as "shock absorbers" between your thighbone and shinbone. They are tough and rubbery to help cushion the joint and keep it stable.
The knee joint is surrounded by a thin lining called the synovial membrane. This membrane releases a fluid that lubricates the cartilage and reduces friction.
Description
With arthritis, over time, and with wear and tear or chronic inflammation the cartilage surface deteriorates and becomes rough. As the cartilage in the knee joint gradually wears away, bone spurs can form along the edges of the joint. The protective space between the bones decreases, and can result in bone rubbing on bone. As the cartilage wears all the way through, the under lying bone begins to grind like sand paper on wood. This is very irritating to the joint and causes inflammation, pain and reduced function.

Symptoms
A knee joint affected by arthritis may be painful and inflamed. Generally, the pain develops gradually over time, although sudden onset is also possible. There are other symptoms, as well:
- The joint may become stiff and swollen, making it difficult to bend and straighten the knee.
- Pain and swelling may be worse in the morning, or after sitting or resting.
- Vigorous activity may cause pain to flare up.
- Loose fragments of cartilage and other tissue can interfere with the smooth motion of joints. The knee may "lock" or "stick" during movement. It may creak, click, snap or make a grinding noise (crepitus).
- Pain may cause a feeling of weakness or buckling in the knee.
- Many people with arthritis note increased joint pain with rainy weather.
When to seek Medical Attention
If you are experiencing these symptoms on a consistent basis, and simple home remedies or over-the counter medications are not providing enough relief, make an appointment. We can help confirm your diagnosis and discuss a treatment plan to help regain your function and mobility.
Examination
During your appointment, your symptoms and medical history will be reviewed. A physical examination will be performed, and x-rays will be reviewed.
Physical Examination
During the physical examination, we will look for:
- Joint swelling, warmth, or redness
- Tenderness about the knee
- Range of passive (assisted) and active (self-directed) motion
- Instability of the joint
- Crepitus (a grating sensation inside the joint) with movement
- Pain when weight is placed on the knee
- Problems with your gait (the way you walk)
- Any signs of injury to the muscles, tendons, and ligaments surrounding the knee
- Involvement of other joints (an indication of rheumatoid arthritis)
Imaging Tests
- X-rays. These imaging tests create detailed pictures of dense structures, like bone. They can help distinguish among various forms of arthritis. X-rays of an arthritic knee may show a narrowing of the joint space, changes in the bone and the formation of bone spurs (osteophytes).
- Other tests. Occasionally, a magnetic resonance imaging (MRI) scan, a computed tomography (CT) scan, or a bone scan may be needed to determine the condition of the bone and soft tissues of your knee.

Treatment
There is no cure for arthritis but there are a number of treatments that may help relieve the pain and disability it can cause.
Nonsurgical Treatment
As with other arthritic conditions, initial treatment of arthritis of the knee is nonsurgical. We may recommend a range of treatment options.
Lifestyle modifications. Some changes in your daily life can protect your knee joint and slow the progress of arthritis.
- Minimize activities that aggravate the condition, such as climbing stairs.
- Switching from high impact activities (like jogging or tennis) to lower impact activities (like swimming or cycling) will put less stress on your knee.
- Losing weight can reduce stress on the knee joint, resulting in less pain and increased function.
Physical therapy. Specific exercises can help increase range of motion and flexibility, as well as help strengthen the muscles in your leg. A physical therapist can help develop an individualized exercise program that meets your needs and lifestyle.
Assistive devices. Using devices such as a cane, wearing shock-absorbing shoes or inserts, or wearing a brace or knee sleeve can be helpful. A brace assists with stability and function, and may be especially helpful if the arthritis is centered on one side of the knee. There are two types of braces that are often used for knee arthritis: An "unloader" brace shifts weight away from the affected portion of the knee, while a "support" brace helps support the entire knee load.
Other remedies. Applying heat or ice, using pain-relieving ointments or creams, or wearing elastic bandages to provide support to the knee may provide some relief from pain.
Medications. Several types of drugs are useful in treating arthritis of the knee. Because people respond differently to medications, we will work closely with you to determine the medications and dosages that are safe and effective for you.
- Over-the-counter, non-narcotic pain relievers and anti-inflammatory medications are usually the first choice of therapy for arthritis of the knee. Acetaminophen (Tylenol) is a simple, over-the-counter pain reliever that can be effective in reducing arthritis pain. Like all medications, over-the-counter pain relievers can cause side effects and interact with other medications you are taking. We will be sure to discuss potential side effects.
- Another type of pain reliever is a nonsteroidal anti-inflammatory drug, or NSAID (pronounced "en-said"). NSAIDs, such as ibuprofen and naproxen (Advil and Aleve), are available both over-the-counter and by prescription.
- A COX-2 inhibitor is a special type of NSAID that may cause fewer gastrointestinal side effects. Common brand names of COX-2 inhibitors include Celebrex (celecoxib) and Mobic (meloxicam, which is a partial COX-2 inhibitor).
- Corticosteroids (also known as cortisone) are powerful anti-inflammatory agents that can be injected into the joint. These injections provide pain relief and reduce inflammation; however, the effects do not last indefinitely. It is recommended that we limit the number of injections to three or four per year, per joint, due to possible side effects.
- Viscosupplementation involves injecting gel into the joint to lubricate and improve the quality of the joint fluid.
- Glucosamine and chondroitin sulfate, substances found naturally in joint cartilage, can be taken as dietary supplements. Although it has not been shown to decrease or reverse the progression of arthritis over time, patient reports indicate that these supplements may relieve pain.
Alternative therapies. Many alternative forms of therapy are unproven, but may be helpful to try, provided you find a qualified practitioner and keep us informed of your decision. Alternative therapies to treat pain include the use of therapies such as acupuncture, and magnetic pulse therapy, CBD among others.
Surgical Treatment
If your pain from arthritis causes disability and is not relieved with nonsurgical treatment surgery may be the next option. As with all surgeries, there are some risks and possible complications with different knee procedures. We will discuss the possible complications with you before your operation.
Arthroscopy. During arthroscopy, we use small incisions and thin instruments to diagnose and treat joint problems. Arthroscopic surgery is not often used to treat arthritis of the knee. In cases where osteoarthritis is accompanied by a meniscus tear, arthroscopic surgery may be recommended to treat the torn meniscus.
Cartilage grafting. Normal, healthy cartilage tissue may be taken from another part of the knee or from a tissue bank to fill a hole in the articular cartilage. This procedure is typically considered only for younger patients who have small areas of cartilage damage.
Osteotomy. In a knee osteotomy, either the tibia (shinbone) or femur (thighbone) is cut and then reshaped to relieve pressure on the knee joint. Knee osteotomy is used when you have early-stage osteoarthritis that has damaged just one side of the knee joint. By shifting your weight off the damaged side of the joint, an osteotomy can relieve pain and significantly improve function in your arthritic knee.
Total or partial knee replacement (arthroplasty). The damaged cartilage and bone is removed, and then new metal or plastic joint surfaces are positioned to restore the function of your knee.

Recovery
After any type of surgery for arthritis of the knee, there is a period of recovery. Recovery time and rehabilitation depends on the type of surgery performed.
Physical therapy is recommended to help you regain strength in your knee and to restore range of motion. Depending upon your procedure, you may need to wear a knee brace, or use crutches or a cane for a time.
In most cases, surgery relieves pain and makes it possible to perform daily activities more easily.
Source: drlatteier.com
